In Conversation With… An interview with Victoria Muir, Pelvic Health Physiotherapist
As part of our series of blogs, meeting the people who work at Bedford Consulting Rooms; BCR’s Helen caught up with Pelvic Health Physiotherapist, Victoria Muir, to find out what inspires her in her work, and all about how the pelvic floor works and what it does for our bodies.
Fact File – Victoria Muir:
• Qualified in 1993 (Birmingham University), and began her career at Bedford NHS Hospital where she set up and developed the Women’s Health and Continence Service (now known as the Pelvic Health Service)
• Completed her diploma in Continence Treatment and Management at the University of East London (1998), and specialised in Male and Female Pelvic Health
• Active member of the Pelvic, Obstetric and Gynaecological Physiotherapy Society (POGP); recently joined the Educational sub-committee
• Member of United Kingdom Continence Society (UKCS), and International Continence Society (ICS).
• Alongside NHS work, has worked privately for more than 20 years providing a specialist Pelvic Health service to both male and female patients.
• Recognising the sensitive and often complex nature of pelvic health conditions; undertook specialist training in the related field of Psychosexual Counselling (2006) to support patients with this aspect of their treatment journey
• Trustee and active member of The Friends of Prostate Sufferers charity support group – FOPS
• Actively fundraises for research into continence management
Helen: What led you into training to be a physiotherapist?
Victoria: I had a background in competitive gymnastics and sports, and so an awareness of the body, as well as an interest in anatomy and physiology. I’d done some voluntary work at the Bristol cancer centre, and from this experience I saw that I was suited to a profession where I could support people in a practical way to address health needs.
I decided to train to become a physiotherapist at the age of 25, after having experienced physiotherapy treatment for my own sports injuries. My mother was a physiotherapist, and she would treat me (or ask one of her colleagues to!); this helped me to understand the body better, and to experience the patient perspective as to how this can improve quality of life, and help a person to regain function, which inspired me to train to be able to do this for others.
Helen: What made you specialise in pelvic health physiotherapy?
Victoria: As a new physiotherapist I worked in many different clinical settings consolidating my training. One theme frequently came up but often wasn’t the ‘reason’ I was initially seeing the patient. It was normally mentioned just as a treatment session came to an end and they were leaving their appointment. It was “by the way…” and then they would mention they were having a bladder or bowel issue.

This could be any clinical setting from young people with sports injuries, in a ward situation following an operation, to new mums presenting with back pain as well as in care of the elderly. Sadly this was often left neglected at the end of the conversation, when it was in fact such an important and impactful thing for a person.
It was evident to me that there were so many people; men and women; had these types of issues but didn’t come forward to ask for help right away like they would for another issue, It was more widespread than many realise, and yet people did not mention it until the end of their appointment, and only then in passing, because there was such a taboo about it and they were embarrassed.
Helen: Why do you think people are embarrassed to talk about pelvic health?
I think it is because historically it has just not been talked about. Somewhat worryingly, it has become normalised in some sectors to have issues with incontinence or pelvic floor, as if it is somehow inevitable or can’t be rectified, which doesn’t help, as it is definitely something that can be addressed and improved with treatment.
I call the muscles of the pelvic floor the “dignity muscles”, because that is what they provide to us when they are working correctly, they give us the independence to go about our lives in the way we want to. When people have issues with continence, they will spend time “toilet-mapping” whilst they are out and about; checking that they’re not going to get caught out. This preoccupation can affect all aspects of their quality of life, and create a level of self-consciousness and lack of confidence.

For this reason, there are many emotional aspects to pelvic health which is why I’m so passionate about working with people to improve that dignity and quality of life.
Helen: Do you think the awareness and profile of pelvic health is improving?
Yes, through TV programmes & social media awareness is improving so people are beginning to talk about continence and other related pelvic health issues but still it is a very hard subject for many to acknowledge or seek treatment. However care and treatment is rapidly improving so it’s important to continue to raise awareness which I try to do , as does my Chartered society and professional specialist clinical group – POGP: Pelvic, Obstetric, Gynaecological Physiotherapy.
Helen: What do you enjoy about being a Pelvic Health Physiotherapist?
Victoria: I think that in order to have a good life you need to have health, and for me it is all about getting people to their optimum health in order to fulfil both their working life, and their social life, and getting people back to function in these things.
Without wishing to blow my own trumpet, I would say this can be life changing for patients; if I can get them back from being at their most vulnerable to being part of the community again, that’s very rewarding.
Helen: For the uninitiated, can you tell us more about what the pelvic floor is made up of, and what it does for us?
Victoria: Yes, it is in I would call the “saddle area”, so in between the legs. Just to note also, that it isn’t the buttock muscles, or abdominal muscles!
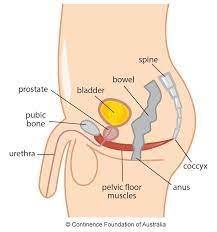
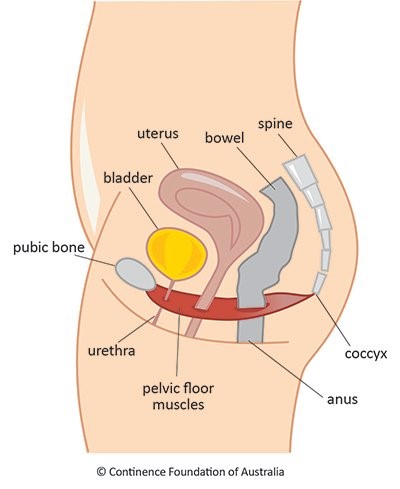
Overall, the pelvic floor is a responsive complex of muscles, which sits below the bowel and bladder and prostate in men and these organs and the womb in women. Because bowel and bladder are those organs that hold the waste matter before excreting it, the wee and the stool both need to move through this muscle complex to exit the body at an appropriate time, and under our conscious control.
The pelvic floor is therefore a responsive muscle complex, responding appropriately to any increased loads placed on it, from the bowel or the bladder above. Causes of increased loads on the pelvic floor can be intraabdominal or intrapelvic, meaning that a sneeze, a cough, physical exercise or exertion (e.g. lifting something heavy) can also place pressure on the pelvic floor, to which it needs to be able to respond.
There are two layers of muscle, the superficial layers that are more of a sphincteric action, and also involved in sexual function; and then the deeper muscular layers that provide closure to the anus and urethra and support the organs above them.
Helen: Many people will have heard of pelvic floor exercises, but as you describe it the pelvic floor is more complex than just squeezing to stop a wee?
Victoria: The pelvic floor is a skeletal muscle just like those of the arms and in the legs, which therefore means that it can be exercised, and therefore that its strength and function can be improved.
However, we must be cautious about old bits of misinformation that have gone around in the past, for example the idea that stopping urination in mid flow can somehow help the pelvic floor, (please don’t do this!). Whilst these pelvic floor muscles are involved in this action, this is not a good way to exercise them. For both men and women, the action of tightening the muscles around the anus and water pipe and drawing up – or “squeeze and lift” – is the way to begin to exercise, but we know from the research is that many people cannot do this themselves in the correct way, and that they therefore need to be examined by a specially trained practitioner to ensure they are doing this correctly.
There is also something to be said about the psychological aspect and the way we think, and connect the brain with muscles, the holistic aspect of neurophysiology, because in a way the brain pelvic connection can be neglected; so re-establishing this conscious connection is part of the overall approach.
See Pelvic Health Physiotherapy in action in Victoria’s video (right) in which the patient is very happy to help demonstrate with a lifting exercise.
Helen: What sort of symptoms would respond to pelvic floor health physiotherapy?
The types of issues that I deal with can be those where people are experiencing bladder and bowel control problems, such as where they can’t hold their wee or poo in, and have to dash to the loo; or for example Stress Urinary Leakage, where a sneeze or cough, or putting pressure into the tummy and down into the pelvic floor, such as with heavy lifting can mean that they get urine, stool or wind leakage.
Women who have given birth may also experience issues with the pelvic floor due to the pressure placed on this and the pelvic organs during their pregnancy and from childbirth. This can lead to the feeling that things are going to ‘fall out of them’ and can be very frightening as well as affect the pelvic organ function. Sometimes people also experience chronic pelvic pain for many different reasons. For men who have had surgery for prostate issues, this can cause continence issues because the prostate sits around the water pipe and affect urine flow and due to scarring which can cause pain and difficulties with passing urine.

Helen: At the beginning of the interview you mentioned sport, do you still get involved in sporting activities?
Victoria: Yes, I enjoy running and cycling, and I have used these also to fundraise for research into continence management.
The fund raising was for the Parnell Fund – University College Hospital London and by half marathons run for this charity. This year we will be cycling through Sardinia.
Helen: Thank you for taking the time to speak to me today!
Victoria works on Mondays, Wednesdays and Fridays at Bedford Consulting Rooms. Send her a message via the contact form on her webpage, to find out more about how she may be able to help you if you are experiencing the types of issues we’ve talked about above.
Research, Conferences and Media:
• 2002: Victoria co-authored an award winning, county-wide programme of study days and a Continence Training Pack for GP’s and midwives; following on from her team’s multidisciplinary patient-centred research ‘Three Counties Continence Project
•2013, Victoria organised and presented at the ‘Current Issues In Continence Management’ study day alongside recognised experts in the field, s an executive member of the Chartered Physiotherapists Promoting Continence (CPPC)
• Victoria was interviewed on BBC Three Counties Radio on Nana Akua’s Live Health Show; she spoke about the importance of continence problems no longer being seen as a taboo subject but a condition that can respond to treatment and should be discussed routinely



